A Guide to Understanding & Managing the Condition
Polycystic Ovary Syndrome (PCOS) is a prevalent hormonal disorder that affects women of reproductive age, but its exact cause remains unclear and is often misunderstood. Characterised by a range of symptoms, including irregular menstrual cycles, excessive hair growth, acne, and weight gain, PCOS can significantly impact a woman’s quality of life. The prevalence of PCOS varies widely, affecting approximately 6% to 21% of women, depending on the diagnostic criteria used and the population studied.

This condition is particularly common among those who are overweight or obese, making it crucial to understand its implications and management strategies.
Symptoms & Diagnosis
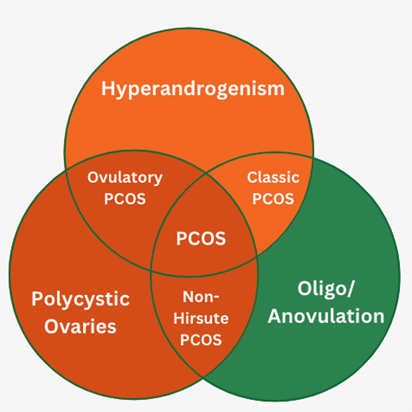
Diagnosing PCOS typically requires the presence of at least two of the following criteria: irregular or absent menstrual periods, signs of excess androgen (such as hirsutism or acne), and polycystic ovaries visible on an ultrasound. The symptoms can vary greatly among individuals, leading to a wide range of experiences. Many women with PCOS also face challenges related to fertility, as the condition can disrupt ovulation. Early diagnosis and intervention are essential to manage symptoms effectively and reduce the risk of long-term complications, such as type 2 diabetes and cardiovascular disease. Additionally, PCOS has also been shown to have psychological implications, such as anxiety, depression and an overall lower quality of life.
Insulin Resistance & PCOS
Insulin resistance is a significant factor in the development and management of PCOS. Many women with this condition experience elevated insulin levels, which can lead to weight gain and intensified symptoms. Strategies to improve insulin sensitivity include regular physical activity, particularly resistance training and high-intensity interval training (HIIT). These forms of exercise not only help with weight management but also enhance glucose metabolism, making them effective tools for managing PCOS.
Diet & PCOS
Diet plays a crucial role in managing the symptoms of Polycystic Ovary Syndrome (PCOS), with the primary objective being the reduction of insulin resistance to improve overall health markers. Lifestyle changes are essential in this management approach, particularly through regular physical activity which can significantly enhance insulin sensitivity and support weight loss.
Protein intake is particularly beneficial for women with PCOS, as they often experience metabolic inflexibility, leading to increased protein oxidation during overnight fasts and reduced fat oxidation. A higher protein diet is well-documented for its effectiveness in aiding weight loss and improving body composition. Consuming protein before bedtime can also be advantageous, as it may help mitigate protein oxidation, addressing the metabolic challenges faced by those with PCOS.
While the optimal balance between carbohydrates and fats remains somewhat unclear, both moderate fat intake and carbohydrate restriction have been shown to be effective in maintaining weight loss and enhancing reproductive and metabolic health. Research suggests that adopting a diet low in glycaemic index (GI) and high in protein can further improve insulin sensitivity and promote weight loss.

Focusing on whole foods, such as fruits, vegetables, lean proteins, and healthy fats, supports overall health and well-being. These nutrient-dense foods help stabilise blood sugar levels, which is particularly important for women with PCOS. By implementing these dietary strategies and lifestyle changes, women can take proactive steps toward managing their condition and enhancing their overall health.
Supplementation
In addition to dietary changes and exercise, certain supplements may support women with PCOS. Key options include Vitamin D, omega-3 fatty acids (EPA and DHA), L-carnitine, and myo-inositol, which have been studied for their benefits in enhancing insulin sensitivity and metabolic health.
Omega-3 Fatty Acids
- Benefits: Omega-3 supplements have been shown to help balance hormones, improve lipid profiles, reduce liver fat, and lower blood pressure compared to a placebo. A daily intake of 1.2g of EPA and DHA can enhance adiponectin levels (hormone produced by fat cells that helps regulate glucose levels and fatty acid breakdown) and reduce insulin resistance.
- Dosage: 2-3g of combined EPA and DHA daily, adjusting based on oily fish intake. Algae supplements are suitable alternatives for vegetarians and vegans.
Vitamin D
- Benefits: Vitamin D is linked to insulin resistance and Type 2 Diabetes risk. Low levels correlate with higher fasting glucose and insulin levels, while higher levels are associated with improved insulin sensitivity.
- Dosage: Testing should be conducted to confirm vitamin D levels above 75nmol/L (30ng/mL). In cases where testing is not feasible, daily intake should not exceed 4000 IUs, and it should be taken with fats to enhance absorption.
L-Carnitine
- Benefits: In clinical trials, L-carnitine significantly improved weight loss, reduced waist and hip circumference, and lowered fasting glucose and insulin levels.
- Dosage: The above research used a daily dose of 250mg, taken with the highest carbohydrate/protein meal.
Myo-Inositol
- Benefits: Myo-inositol has been shown to enhance ovarian function and lower testosterone and insulin levels in women with PCOS.
- Dosage: Recommended intake is 2-6g per day, divided into two doses (morning and evening), for at least 6 months, with some noticing results sooner.
These supplements may help women with PCOS manage their condition more effectively. Always consult a healthcare provider before starting any new supplementation.
Metabolic Implications
Managing PCOS can be particularly challenging due to significant metabolic implications. Women with PCOS often experience a reduced ability to burn calories after meals and may have a basal metabolic rate that is up to 40% lower than that of women without the condition. This metabolic adaptation means that they frequently require more aggressive dieting strategies to achieve weight loss, making the process more difficult to adhere to.
Additionally, women with PCOS typically have a diminished release of the hormone cholecystokinin (CCK) after meals. This hormonal difference can hinder their ability to feel satiated, leading to persistent hunger even after eating. This appetite regulation issue is further exacerbated by elevated testosterone levels, which are common in women with PCOS, complicating their efforts to manage weight effectively.

Research suggests that intermittent fasting may offer a more effective alternative to daily calorie restriction for enhancing insulin sensitivity and reducing body fat in overweight women. This approach holds promise for improving metabolic health in women with PCOS, but the inherent challenges of the condition make it clear that managing PCOS requires a multifaceted approach.
Tips for Managing PCOS
Managing Polycystic Ovary Syndrome (PCOS) can be challenging, but there are several practical strategies that can improve health outcomes. Here are some effective tips to consider:
- Adopt a MUFA-Enriched Diet: Incorporating monounsaturated fats (MUFA) can aid in weight loss, whilst allowing for a moderate consumption of saturated fats.
- Consider a Low-GI Diet: Focusing on low-glycemic index (GI) foods can enhance menstrual regularity, reduce insulin resistance, and improve cholesterol levels.
- Incorporate a High-Protein Diet: A diet high in protein can improve mood, boost self-esteem, and assist with weight loss. Consuming about 15% of total daily calories from fruit helps reduce protein oxidation.
- Aim for Weight Loss if Overweight: Weight loss is often linked to improved PCOS symptoms, regardless of dietary approach.
- Focus on a Balanced Diet: Prioritising a diet rich in whole foods, including a variety of fruits, vegetables, lean proteins, and healthy fats supports overall health.
- Stay Active: Regular physical activity, including both cardiovascular and strength training, will enhance insulin sensitivity and weight management.
- Monitor Symptoms: Tracking menstrual cycle and bodily changes can be valuable for communicating with healthcare providers.
- Consider Supplementation: Discuss supplements like myo-inositol, vitamin D, Carnitine, and omega-3 fatty acids with a healthcare provider.
- Seek Support: Joining PCOS support groups or online communities can provide valuable shared experiences and tips.
- Consult a Professional: Partner with a healthcare provider knowledgeable about PCOS to create a personalised management plan tailored to individual needs.
Implementing these strategies can support the management of PCOS and contribute to overall well-being.
Conclusion
Polycystic ovary syndrome (PCOS) is a complex condition that necessitates a comprehensive management approach. While research findings on PCOS can vary, one consistent conclusion is that weight loss is beneficial for women with this condition, regardless of the specific dietary approach employed. This underscores the importance of individualised weight loss programmes that cater to each person’s unique needs.
Additionally, testing for vitamin D deficiency is recommended for women with PCOS, and further research is warranted to investigate the potential benefits of omega-3 fatty acid supplementation (EPA and DHA). Diets characterised by low glycaemic index/load (GI/GL) and high in monounsaturated fats (MUFA) have shown promise in promoting weight loss, improving menstrual regularity, reducing insulin resistance, and enhancing overall quality of life, including better management of mood and self-esteem.
By understanding the symptoms, implementing healthy dietary changes, enhancing insulin sensitivity, and considering appropriate supplementation, women with PCOS can take significant steps toward improving their health.

Collaborating with a nutritionist can help identify the most effective strategies tailored to individual circumstances. With the right support and tailored strategies, it is possible to address the challenges associated with PCOS and lead a fulfilling life.
References
- MacDonald, M. (n.d.). Lecture on Understanding the Signs, Symptoms & Implications for PCOS, Mac Nutrition Uni.
- Giacco, R., et al. (2007). Omega-3 supplementation and its effects on insulin sensitivity.
- Phelan, N., et al. (2011). Hormonal and lipid modulation in women with PCOS.
- Cussons, A., et al. (2009). The impact of omega-3 supplementation on liver fat and blood pressure in PCOS patients.
- Mohammadi, M., et al. (2012). Effects of EPA and DHA supplementation in women with PCOS.
- Vargas, A., et al. (2011). The differential effects of omega-3 fatty acids in the context of PCOS.
- Kotsa, K., et al. (2009). The role of vitamin D supplementation in managing PCOS.
- Diamanti-Kandarakis, E., & Papavassiliou, E. (2006). Molecular mechanisms of insulin resistance in polycystic ovary syndrome.
- Alvarez-Blasco, F., et al. (2006). Prevalence and characteristics of polycystic ovary syndrome in overweight and obese women.
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. (2004). Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome.
- Foreyt, J. P., et al. (2004). Weight-reducing diets: Are there any differences?
- Moran, L. J., et al. (2003). Dietary composition in restoring reproductive and metabolic physiology in overweight women with polycystic ovary syndrome.
- Naude, W. A., et al. (2014). Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: A systematic review and meta-analysis.
- Kaufman, S. R., et al. (2002). Polycystic ovarian syndrome and insulin resistance in white and Mexican American women: A comparison of two distinct populations.
- Robinson, S., et al. (1993). The relationship of insulin insensitivity to menstrual patterns in women with hyperandrogenism and polycystic ovaries.
- Dunaif, A., et al. (1992). Evidence for distinctive and intrinsic defects in insulin action in polycystic ovary syndrome.
- Moran, L. J., et al. (2013). Dietary composition in the treatment of polycystic ovary syndrome: A systematic review to inform evidence-based guidelines.
- Rodriguez, N. R., et al. (2005). Effects of two energy-restricted diets containing different amounts of fruit on body weight loss and macronutrient oxidation.
- Whigham, L. D., et al. (2014). Metabolic evidence of diminished lipid oxidation in women with polycystic ovary syndrome.
- Marsh, K., et al. (2010). Effect of a low glycemic index diet compared with a conventional healthy diet on polycystic ovary syndrome.
- Stamets, K., et al. (2004). A randomized trial of the effects of two types of short-term hypocaloric diets on weight loss in women with polycystic ovary syndrome.
- Leidy, H. J., et al. (2015). The role of protein in weight loss and maintenance.
- LeCheminant, J. D., et al. (2007). Comparison of a low carbohydrate and low fat diet for weight maintenance in overweight or obese adults enrolled in a clinical weight management program.
- McClain, A. C., et al. (2013). Adherence to a low-fat versus low-carbohydrate diet differs by insulin resistance status among overweight adults.
- Cornier, M. A., et al. (2005). Insulin sensitivity determines the effectiveness of dietary macronutrient composition on weight loss in obese women.
- Pittas, A. G., et al. (2005). A low-glycemic load diet facilitates greater weight loss in overweight adults with high insulin secretion but not in those with low insulin secretion in the CALERIE trial.
- Gardner, C. D., et al. (2016). Weight loss on low-fat vs. low-carbohydrate diets by insulin resistance status among overweight adults: A randomized pilot trial.
- Pittas, A. G., et al. (2006). Vitamin D and calcium intake in relation to type 2 diabetes in women.
- Chiu, K. C., et al. (2004). Hypovitaminosis D is associated with insulin resistance and beta-cell dysfunction in nondiabetic subjects.
Main – Photo by RDNE Stock project



