…In Inflammatory Diseases
“The smallest one is not always the one we think“
Microbiota, Intestinal flora, Microbioma, Dysbiosis, Chronic inflammation, Para-inflammation, Innate immunity, Adaptive immunity, Metabolism, Neurological diseases, Natural therapeutic treatments
At the crossroads between modern medicine and the mysteries of the body, the role of the microbiota is a microscopic ecosystem that resides in us. This paper highlights the complex interaction between the microbiota and our health, paving the way for new strategies to prevent and treat inflammatory diseases from a holistic perspective.

Addressing concepts such as dysbiosis, innate and adaptive immunity, and metabolism, this paper highlights how the imbalance of our gut flora can lead to various pathologies, from metabolic disorders to neurological diseases. In addition, it examines natural therapeutic approaches to restore microbiota balance, highlighting the importance of a balanced diet, deficiencies, exercise, and stress management.
I – What Is The Microbiota?
The microbiota, commonly called microbial flora, encompasses all the microorganisms that colonize a particular environment, such as the human body. At the same time, the microbiome represents all the genes within these microorganisms, thus encompassing their genetic diversity.
The human gut microbiota is a complex ecosystem of billions of bacteria, viruses, parasites, and fungi. It would be about 2 kg, heavier than the brain. Our bodies comprise more microbes than human cells (we harbor about 40,000 billion bacteria in our large intestine, along with viruses and fungi). According to a study conducted by Ursell et al. (2012) [1], the composition of the microbiota varies according to various factors such as age, diet, and state of health. It is a dynamic and balanced ecosystem that plays a crucial role in many biological processes, including digestion, metabolism, and immunity.
The researchers found that the bacterial diversity of the microbiota is essential for maintaining intestinal health. A study conducted by Lozupone and Knight (2007) [2] has shown that people with inflammatory bowel disease (IBD) have reduced bacterial diversity in their gut microbiota compared to healthy individuals. This research underscores the importance of maintaining a balanced microbiota to prevent inflammatory diseases.
The microbiota is mainly located in the small intestine and the colon, distributed between the lumen of the digestive tract and the protective biofilm formed by the intestinal mucus that covers its inner wall. Because stomach acid does not support the presence of most microorganisms, the stomach contains one hundred million times less commensal bacteria than the large intestine. This geographical distribution of the microbiota is crucial for its optimal functioning.
The enteric nervous system is closely related to the immune system. Our three homeostasis systems are the nervous/neurological system, immune system, and endocrine system, which are orchestrated by our digestive system, which is at the center. Genetic inheritance would account for only 1% of genes, with the remaining 99% mainly acquired from the immediate environment at birth, including the birth canal and breast milk (Annalisa N, Alessio T, Claudette TD, Erald V, Antonino DL, Nicola DD, 2014) [3]. This would result in the most abundant and most biodiverse colon ecosystem.

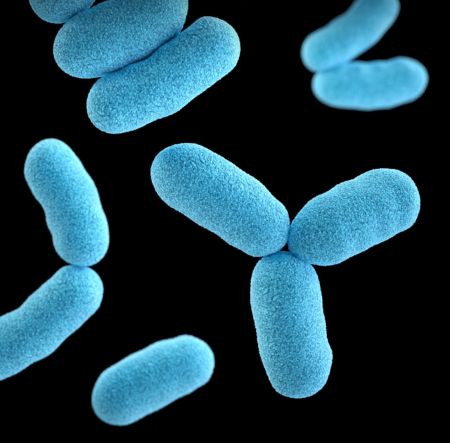
We also harbor billions of bacteria and other microorganisms outside the gut (mouth, skin, vagina, urinary tract, respiratory tract). Our microbiota is our own (of varying richness; our intestinal microbiota is unique; it is different in each individual). The bacteria are grouped into 3 large families called “phyla”, among which the 3 major ones are Firmicutes, Bacteroidetes, and Actinobacteria. Within these large families, we find the lactobacilli (Lactobacillus) in the form of rods or the bifidobacteria (Bifidobacterium) in the form of Y, then also the Bacteroides, Ruminococcus, and Prevotella.
A very ancient symbiotic relationship exists between us and our microbiota. It is important to remember that microbes were present on Earth before us; they live within us and are essential to the proper functioning of our bodies. This symbiosis is mutualistic because the human and his microbiota benefit from their relationship. If we schematize, a good diet plus a healthy lifestyle = our intestinal bacteria help us to digest fiber, synthesize many metabolites like vitamins or neurotransmitters, develop our immune system, and, in fact, protect us from the many pathogens to which we are constantly exposed.
This symbiotic relationship is the key to overall good health. However, this balance is fragile because we are exposed daily to the harmful elements of our microbiota (antibiotics and other drugs, pesticides, alcohol, and even excessive hygiene.). All this can alter it and thus reduce our microbial richness and consequently alter our good health. Dysbiosis appears and becomes the nest of many chronic dysimmunity diseases (disruption of the immune system, T1 diabetes, multiple sclerosis, Crohn’s disease) but also metabolic (T2 diabetes, obesity, hypercholesterolemia) or even cancerous.
The birth of the microbiota in the fetus and then the infant is crucial. Early on, the embryo comes into contact with maternal bacteria in utero, which pass through the placenta in small amounts and cause the body to contact the outside world. During delivery, the newborn will again be in contact with another bacterial world, first that of the vaginal flora of his mother, then with the aerial bacteria present in the delivery room (hence the importance of a natural or cesarean delivery).
Bacteria are born from light, they are the building blocks of an individual and all life. Our microbiota is born during the 1st trimester of pregnancy when the placenta is not yet functional. This first microbiota is linked to that of the mother’s mouth = our 1st intestinal microbiota is meconial (in the meconium and eliminated with the first stool of the new-
born after birth). Unsuitable flora in the child’s first 20 days of life will result in an immunocompromised environment.
At birth, the neonate will be in contact with ambient oxygen through breathing and the mouth. Its intestinal flora will become aerobic and anaerobic. By the 3rd day of life, this flora will again become anaerobic. On day 21, she must rebalance to acquire adult flora between the 18th and the 24th month of life.
Let us remember here that the intestinal flora will be balanced if the intestinal neurological system (enteric nervous system) works in harmony with the intestines.
A – What Is The Role Of The Microbiota?
The microbiota fulfills four main roles:
1 – Metabolic Role:
The microbiota is involved in the differentiation and proliferation of intestinal epithelial cells. It makes it possible to synthesize vitamins, ferment non-digestible food residues, and produce short-chain fatty acids, which are anticancer and anti-inflammatory.
2 – Role Of barrier:
The presence of aerated junctions mediates the induction of Immunoglobulin A (IgA). Finally, thanks to antimicrobial peptides.
3 – Role Of Defense:
Microbiota competes with pathogens (e.g. nutrients), it produces antimicrobial factors (e.g. bacteriocins).
4 – A Maintenance Role:
The immune system develops in the intestinal mucosa, specifically where adaptive immune maturation (eg, Treg) occurs.
B – Function Of The Microbiota In The Digestion
The microbiota plays a crucial role in digestion by contributing to the degradation of food and the absorption of essential nutrients. The main functions of the microbiota in digestion are Fermentation of non-digestible food substrates and residues, such as fiber, short-chain fatty acids (SCFAs), butyrate, and inulin. This fermentation produces metabolites that are beneficial for intestinal health. Facilitate nutrient uptake through a set of enzymes that the body does not have. These enzymes help break down complex food components such as starch, cellulose, and polysaccharides into simpler molecules, thus promoting their absorption by the body.

Participation in synthesizing certain essential vitamins, such as vitamin K, vitamin B12, and vitamin B8. These vitamins are necessary for many biological processes, including blood clotting, carbohydrate metabolism, and fatty acid synthesis. Regulation of several metabolic pathways, including absorption of fatty acids, calcium, and
magnesium. This regulation contributes to maintaining electrolyte balance and bone health.
C- Function Of The Microbiota In The Intestinal Immunity
The gut microbiota plays an essential role in the development and functioning of the intestinal immune system. From the first years of life, the microbiota is necessary for intestinal immunity to learn to distinguish between friendly (commensal) and pathogenic species. This learning ability is crucial for developing an adequate immune response against pathogens.
The microbiota fully participates in the functioning of the intestinal immune system, which is indispensable to the role of the intestinal wall as a barrier. This barrier is constantly exposed to a flow of food or microbial-origin antigens.
Bacteria such as Escherichia coli are directly involved in the fight against the colonization of the digestive tract by pathogenic species in competition with them and by producing bactericidal substances, such as bacteriocins.
In addition, the gut microbiota influences the immune response by producing pro-inflammatory cytokines, which can modulate inflammation and help defend against pathogens.