And What We Could Do Instead
Fibromyalgia: A Brief History
Let’s begin this fibromyalgia fact-check with a history recap. The term rheumatism was first used by the physician Guillaume Baillou in 1592 to describe musculoskeletal pain that didn’t result from injury. In 1815 Scottish surgeon William Balfour was the first to describe the tender points, which are still used to diagnose fibromyalgia today. The term fibrositis was coined by British neurologist William Gowers in 1904 and was not changed to fibromyalgia until 1976. The connection between fibromyalgia and other commonly associated conditions was suggested in 1984. ¹
Today (anno 2023), the condition and treatment are still widely debated. There is no consensus about either cause or treatment, and sufferers are regularly met with scepticism by healthcare professionals because of the lack of structural damage seen in physical tests.
Diagnosis and FIQR
Let us move on to the diagnosis. I have looked at several healthcare organisations to see what they say about how fibromyalgia is diagnosed and wanted to display them next to each other in the hope for clarity:
- Fibromyalgia is diagnosed based primarily on having pain all over the body, along with other symptoms. Currently, there are no specific laboratory or imaging tests for fibromyalgia. The main symptoms—pain and fatigue—are shared with many other conditions, so doctors typically try to rule out other causes for your symptoms. (NIH, NIAMS) ²
- Diagnosing fibromyalgia can be difficult as there’s no specific test to diagnose the condition. The symptoms of fibromyalgia can also vary from person to person. (NHS) ³
- In the past, doctors would check 18 specific points on a person’s body to see how many of them were painful when pressed firmly. Newer guidelines from the American College of Rheumatology don’t require a tender point exam. Instead, the main factor needed for a fibromyalgia diagnosis is widespread pain throughout your body for at least three months. (Mayo Clinic)⁴, (ACR) ⁵
- Doctors usually diagnose fibromyalgia using the patient’s history, physical examination, X-rays, and blood work. (CDC) ⁶
- Fibromyalgia is diagnosed with a careful history, a physical examination, as well as a symptom questionnaire based on the diagnostic criteria, and appropriate blood tests to exclude other or diagnose coexisting conditions (Fibromyalgia Australia) ⁷
These are only a few descriptions, but they do roughly say the same: “The patient is in pain, the pain is all over the body, it has lasted longer than 3 months, we’ve run all the tests but cannot find a structural reason… Diagnosis must be fibromyalgia”. This might sound a bit blunt, but for someone who is working in a field that is often criticised for being too Woo-woo or unscientific (read: any type of holistic or alternative healing), I am struggling to see how this diagnosis has come to be widely accepted.
Moving on, let’s have a look at the FIQR (the Revised Fibromyalgia Impact Questionnaire (2009)), which is used to measure the severity of the impact of fibromyalgia on the lives of sufferers. The questionnaire includes a list of physical activities (climbing stairs, vacuuming, walking, doing groceries) where the patient indicates the difficulty level on a scale of 1-10.

Followingly, they are asked whether they felt fibromyalgia prevented them from achieving their goals in the last week, and to what extent they felt overwhelmed, also on a 10-point scale. Finally, there is a list of questions to indicate: pain level, sleep quality, energy level, and level of depression (among a few others).
These questions are not irrelevant, quite the contrary, especially since the goal is to measure the impact of fibromyalgia on their lives, and yes, the impact is mostly physical, indeed.
But instead of asking how they feel, they are only asked to what extent they feel overwhelmed and depressed, as if those are the only two options.
Looking at the overall questionnaire, it becomes apparent that the focus is almost purely physical, overlooking crucial areas that impact our health.
The Biomedical vs. Biopsychosocial Model
This brings me to the next issue: our biomedical healthcare model. Our Western biomedical model looks at the human body like a mechanic looks at a damaged car, where the broken parts can either be mended or replaced. Humans, though, are a little more complex than that, and there are other factors that play a fundamental role in our health.
We now know that, what we believe and feel in our mind, can be felt in the body, and that emotions like fear can trigger an avalanche of responses in our nervous system, setting in motion a number of physical responses. All based on a feeling we experience, whether we are facing a direct threat or not. Vice versa, there has been research done into how movement helps alleviate depression, how ‘power poses’ can help increase self-esteem, and how forcing a smile on your face, can actually generate happiness chemicals.

The Mindbody connection is undeniably strong, yet here we are, poking and prodding a person suffering from a chronic condition while not finding any answers, yet also not looking beyond the physical body. I cannot understand the science of this!
Luckily, there is a wave of physicians pushing for a more holistic model, a biopsychosocial approach, which includes the biological, as well as a person’s psychological state and social environment.
This gives a more complete picture of a person’s health and can lead to a more effective treatment, especially in the case of fibromyalgia.
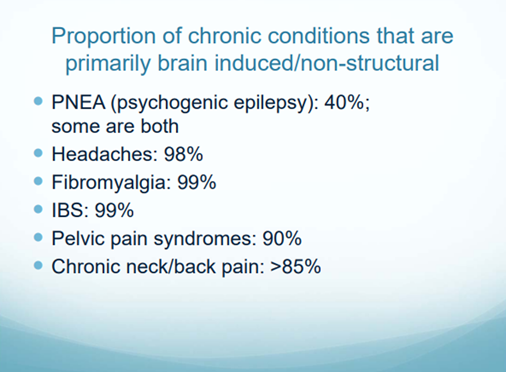
In an earlier article (A Holistic Approach to Chronic Pain), I referred to a presentation of Dr. Howard Schubiner at OptumHealth Education (OHE), in which he presented that many chronic pain conditions have been proven to be primarily brain-induced. Fibromyalgia holds the high score of 99%. ⁸ ⁹ And yet, the main treatment is still based on a biomedical approach.
Medications and their effectiveness
Now over to the fun part, let’s talk about the even more controversial topic of medication, one of the (if not THE) main treatments for fibromyalgia pain. There are several, and according to research done with over 2,500 fibromyalgia sufferers, 74% reported spending between 100 – 500 USD a month on medication.¹⁰ But how effective are they?
The same research asked the participants to rate whether the medication was considered helpful. The highest rated 5 were Vicodin (75%), Xanax (70%), Oxycodone (67%), Valium (65%) Ambien (64%). Sounds promising right? But what do they all have in common? They all fall in the category of benzodiazepines, a group of depressant drugs, which numbs the symptoms, masking them, NOT removing them. Patients need to keep taking them, swallowing them with their side effects, and run the risk of becoming addicted. How is this called “treatment”?

A more recent research on fibromyalgia, published in March 2018, stated that “contrary to common belief, the effect of these FDA-approved drugs is less than satisfactory”. ¹¹
Mindbody treatments
I might be biased, since I’m working in the field of Mindbody healing, yet, having read the cases of people who can call themselves pain-free on forums such as TMS wiki, Curable, the Thank You Sarno page, and having seen the same results with my own clients, it isn’t a matter of my opinion. When we broaden the spectrum and look at a person through a biopsychosocial lens, it gives us so many more answers. This not only helps us understand a person’s pain, it helps them understand their own pain.
Many of the patients from Dr. Sarno reported feeling a reduction of symptoms, simply by understanding what was causing the pain, which can be: repressed emotions such as anger, grief, or other inner tension caused by daily stress or fears. All these triggers from our thoughts and environment can send our nervous system into overdrive, and send pain signals flying through our bodies, causing immense physical pain. It might be hard to believe that the cause isn’t found in the body, but is it really that hard to believe we are complex beings? That we aren’t just bags of meat that are deteriorating at different speeds?
The modalities that have been proven to be most effective for these types of pain are Mindbody practices, combining talk therapy, breathwork, meditation, movement, lifestyle changes, healthy food, and most importantly education.
Understanding how our body functions, how our brain interacts with our nervous system, and how this affects our pain is a crucial first step.
Then all the other exercises suddenly make sense. When a person knows how and when to apply these, they are set for life. Most of these techniques are free, and best of all, there are no scary side effects.
I would love to share the statistics on Mindbody treatments, but here I could not find any large-scale research, which is probably due to a lack of funding. My personal opinion is that there is no money to be made when people become pain-free, especially through modalities that are, in fact, available for free (such as breath, movement, meditation, and other forms of tension release).

All I know is that the people who have found their way to healing, and call themselves pain-free, report they were able to achieve this through Mindbody methods. So regardless of sample size, or one-size-fits-all treatments, I think these outcomes are worth a spotlight. Let’s look at what has been effective, and stop hiding behind clinical trials, and governmental approval. That might be relevant when there are scary side-effects involved. But please tell me what are the scary side-effects of the Mindbody modalities? Who are we protecting really by not giving these modalities the centre stage? And from what?
Sources
- https://www.verywellhealth.com/the-history-of-fibromyalgia-716153
- https://www.niams.nih.gov/health-topics/fibromyalgia/diagnosis-treatment-and-steps-to-take
- https://www.nhs.uk/conditions/fibromyalgia/diagnosis/
- https://www.mayoclinic.org/diseases-conditions/fibromyalgia/diagnosis-treatment/drc-20354785
- https://rheumatology.org/patients/fibromyalgia
- https://www.cdc.gov/arthritis/basics/fibromyalgia.htm
- https://fibromyalgiaaustralia.org.au/patients/understanding-diagnosis-2/
- https://www.optumhealtheducation.com/sites/default/files/191205-Chronic-Pain-Schubiner-Slides.pdf
- https://www.emedevents.com/online-cme-courses/webcasts/chronic-pain-reconsidered-the-role-of-neural-circuits-in-the-brain
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1829161/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6016048/